Background:
Monoclonal Gammopathy of Renal Significance (MGRS) is a category of diseases not meeting criteria for cancer, in which a clonal population of B-lymphoid or plasma cells produces a nephrotoxic protein leading to kidney injury. Informal consensus has arisen that therapy targeting the causal clone is most likely to be efficacious, and the primary goal of therapy is to prolong renal survival. Light chain (AL) amyloidosis has been extensively studied, yet there is a paucity of data describing outcomes associated with clone-directed therapy for the various subtypes of non-AL MGRS.
Methods:
This was a retrospective analysis of patients treated at two National Cancer Institute (NCI)-designated cancer centers in the United States. Medical records of adult patients seen between January 2010 and March 2023 were screened for MGRS. Patients were eligible if they had renal biopsy-confirmed histopathologic findings compatible with MGRS. AL amyloidosis was excluded. The primary outcome was renal survival, defined as time from diagnosis of MGRS to requiring renal replacement therapy (RRT) or renal transplant, with patients censored at last follow up or death. Baseline characteristics were described, including 24-hour proteinuria, estimated glomerular filtration rate (eGFR), whether a clonal population of B cells or plasma cells could be identified on histopathologic examination of marrow or lymph node biopsy, concentration of monoclonal protein, and involved serum free light chain concentration. Initial therapy was reported, although differences in outcomes across therapeutic strategies were not compared. Baseline clinical characteristics between patients who required RRT and those who did not were compared. Baseline clinical variables and time to RRT were compared across the two most common MGRS subtypes in the cohort: proliferative glomerulonephritis with monoclonal immunoglobulin deposits (PGNMID) and light chain deposition disease (LCDD). Continuous variables were compared across subgroups using Wilcoxon rank-sum test. Time-to-event outcomes were analyzed according to the Kaplan-Meier method. All analyses were conducted using R version 3.6.1.
Results:
In total, 65 patients were included, 23 (35%) of whom ultimately required RRT or transplant. Four patients died, all after RRT. Median baseline proteinuria was 2802 mg/24h (IQR 972.5 - 4492.0) and median eGFR was 33.0 mL/min (IQR 23 - 53) for the entire cohort. In all cases proteinuria was mostly albumin. Median baseline involved light chain concentration was 8.3 mg/dL (IQR 3.1 - 26.4). A majority of patients (n=33, 51%) had no identifiable serum monoclonal protein. The two most common MGRS subtypes were PGNMID (n = 26) followed by LCDD (n = 21). Clonal populations thought to be causing MGRS were identified in 41/64 patients (64%), including 37 (58%) with plasma cell clones, 1 (2%) with a lymphoplasmacytic lymphoma clone, and 3 (4.7%) with other B-cell clones. Clones were not identified in 23 (36%). The most common chemotherapy agents included bortezomib (n=42, 64%) and rituximab (n=14, 22%).
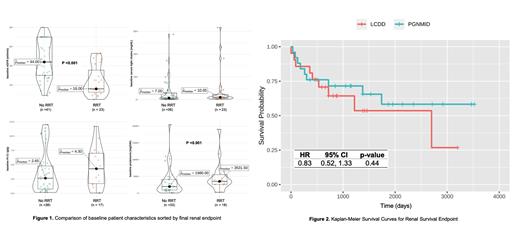
Compared to patients not requiring RRT, patients requiring RRT had higher baseline proteinuria (median 3531 vs. 1980 mg/24h, p<0.001) and lower eGFR (median 16 v. 44 mL/min, p<0.001); differences in serum free light chain concentrations were not significant ( Figure 1). A clonal population thought to be causing MGRS was identified on bone marrow biopsy in a majority of LCDD patients (n = 20, 95%), while clones were infrequently found in PGNMID (n = 6, 23%). The vast majority (n=20, 95%) of patients with LCDD received bortezomib-based therapy. Initial therapy in patients with PGNMID was more evenly divided: 9 (35%) received bortezomib-based therapy, 10 (38%) received rituximab-based therapy, and 6 (23%) received other regimens. Despite differences in therapeutic approach, patients with LCDD and in patients with PGNMID had similar risk of RRT (cumulative risk 35% v. 43%, p=0.54; HR 0.83 (95% CI 0.52-1.33); p =0.44) ( Figure 2).
Conclusion:
Patients with MGRS remain at high risk of requiring RRT even with clone-directed therapy. Despite differences in pathogenic clones and therapeutic strategies, outcomes of patients with PGNMID and LCDD are similar. Because the severity of baseline renal function across MGRS histologies predicts renal survival, early diagnosis and treatment is likely critical to improving renal outcomes.
Disclosures
Jensen:Abbvie: Research Funding. Lentzsch:Alexion Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; Adaptive Biotechnologies: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol Meyers Squibb: Membership on an entity's Board of Directors or advisory committees; Caelum Biosciences: Membership on an entity's Board of Directors or advisory committees, Patents & Royalties: January 1, 2041; Celgene: Research Funding; Clinical Care Options: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees; Karyopharm Therapeutics: Membership on an entity's Board of Directors or advisory committees; Oncopeptide: Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy; Regeneron: Honoraria; Sanofi: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees. Chakraborty:Adaptive Biotech: Consultancy, Honoraria; AbbVie: Research Funding; Genentech: Research Funding; Janssen: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria. Bhutani:Sanofi: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal